Far from being just a feeling, chronic loneliness triggers a cascade of biological responses that can dramatically alter physiological functions, contributing to a range of severe health conditions. Understanding these mechanisms is crucial for both individuals and healthcare professionals seeking to mitigate its detrimental effects.
The Silent Epidemic: Understanding Loneliness and Its Reach
Loneliness is the distressing feeling that arises when a person’s social needs are not met by the quantity or quality of their social relationships. It differs from social isolation, which is an objective lack of social contact. One can be surrounded by people and still feel profoundly lonely, while someone living alone might not experience loneliness if their social needs are fulfilled.

This “silent epidemic” affects millions globally, spanning all age groups, though it’s particularly prevalent among older adults, adolescents, and those facing significant life transitions. Its pervasiveness underscores the urgent need to address its far-reaching consequences on our physical health.
The Biological Pathways: How Loneliness Gets Under Your Skin
The human need for social connection is fundamental, and its absence activates stress responses designed for survival. Loneliness, therefore, isn’t just a psychological state; it’s a physiological threat that triggers specific biological pathways.
Chronic Stress and the HPA Axis
Persistent feelings of loneliness activate the body’s stress response system, specifically the hypothalamic-pituitary-adrenal (HPA) axis. This activation leads to a sustained elevation of stress hormones like cortisol and adrenaline. While acute stress is adaptive, chronic activation of the HPA axis can dysregulate various bodily functions, contributing to numerous physical health issues.
Elevated cortisol levels can disrupt metabolism, suppress the immune system, and increase inflammation, directly impacting several physical health markers over time.
Inflammation: The Body’s Silent Enemy
One of the most significant biological impacts of loneliness is its contribution to chronic inflammation. Studies have shown that lonely individuals often exhibit higher levels of pro-inflammatory markers in their blood, such as C-reactive protein (CRP) and interleukin-6 (IL-6).
This systemic, low-grade inflammation is a cornerstone in the development and progression of many chronic diseases, acting as a silent aggressor that damages tissues and organs throughout the body.
Compromised Immune Function
The chronic stress and inflammation associated with loneliness directly impair the immune system. Research indicates that lonely individuals may have a weaker immune response to vaccines and are more susceptible to infections like the common cold and flu.
Their bodies also show slower wound healing and a reduced ability to fight off pathogens, highlighting a compromised defense system that leaves them more vulnerable to illness.
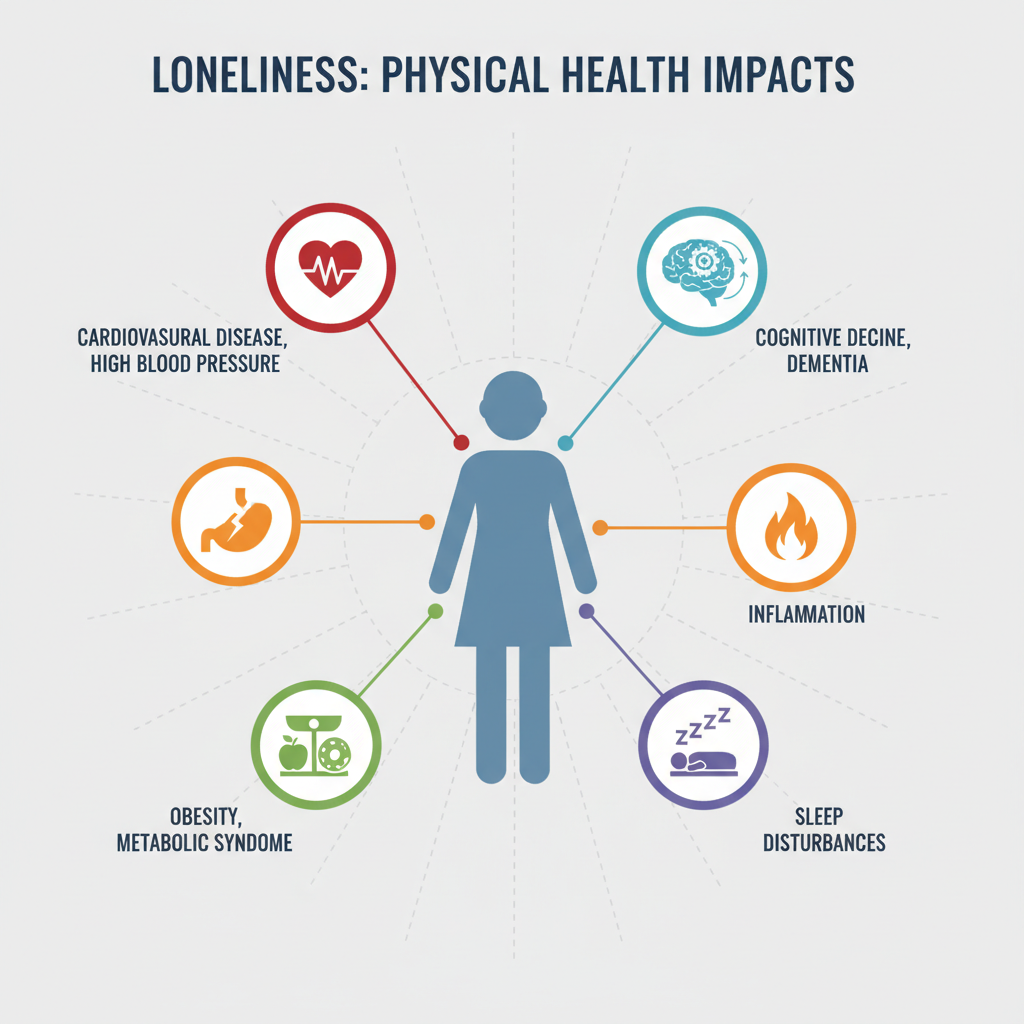
Key Physical Health Markers Affected by Loneliness
The biological pathways activated by loneliness manifest in measurable changes to several crucial physical health markers.
Cardiovascular Health: A Strained Heart
Chronic loneliness significantly elevates the risk of cardiovascular disease. It’s linked to increased blood pressure, a higher resting heart rate, and greater arterial stiffness. These factors place immense strain on the heart and blood vessels, significantly increasing the likelihood of developing hypertension, coronary artery disease, heart attack, and stroke.
The stress hormones and inflammation triggered by loneliness contribute directly to the hardening of arteries and the buildup of plaque, critically impacting heart health markers.
Metabolic Syndrome and Weight Management
Loneliness can disrupt metabolic regulation, contributing to metabolic syndrome. It’s associated with higher rates of obesity, insulin resistance, and an increased risk of type 2 diabetes. This may be partly due to stress-induced changes in eating habits, such as comfort eating and poor dietary choices, alongside reduced physical activity and disrupted sleep patterns often experienced by lonely individuals.
Sleep Disturbances and Fatigue
A strong correlation exists between loneliness and poor sleep quality. Lonely individuals often report difficulty falling asleep, more frequent awakenings during the night, and a less restorative sleep experience. This fragmented sleep further exacerbates stress, inflammation, and metabolic dysregulation, creating a vicious cycle that negatively impacts overall physical health markers and daily energy levels.
Cognitive Decline and Brain Health
The chronic stress, inflammation, and poor sleep associated with loneliness can take a toll on brain health. Studies indicate that loneliness is a risk factor for cognitive decline and is linked to an increased risk of developing dementia, including Alzheimer’s disease. Social interaction is vital for cognitive stimulation, and its absence can lead to reduced cognitive reserve and impaired memory function.
Pain Perception and Chronic Conditions
Loneliness has been shown to alter pain perception, making individuals more sensitive to pain. For those already living with chronic pain conditions like fibromyalgia or arthritis, loneliness can intensify their experience of pain and worsen their overall symptoms. The psychological distress of loneliness can amplify physical discomfort, creating a complex interplay between emotional and physical suffering.
Beyond the Markers: Broader Health Implications
The impact of loneliness extends beyond specific health markers, influencing broader health outcomes. Research consistently demonstrates that chronic loneliness is associated with an increased risk of premature mortality, comparable to well-known risk factors like smoking or obesity.
Furthermore, lonely individuals may be less likely to adhere to medical advice, attend appointments, or engage in health-promoting behaviors, further compounding their health risks and increasing healthcare costs for society.
Building Bridges: Strategies to Combat Loneliness for Better Health
Recognizing the profound impact of loneliness on physical health markers, proactive strategies are essential for improving well-being:
- Foster Meaningful Social Connections: Actively seek out opportunities for genuine interaction. Join clubs, volunteer, engage in community activities, or reconnect with old friends and family. Quality over quantity is key.
- Nurture Existing Relationships: Invest time and effort into maintaining and deepening current friendships and family bonds. Regular communication and shared activities can strengthen these vital connections.
- Seek Professional Support: If loneliness feels overwhelming or persistent, professional help from therapists or counselors can provide coping strategies, address underlying issues, and facilitate social engagement.
- Practice Self-Compassion: Be kind to yourself. Loneliness is a common human experience, not a personal failing. Engaging in self-care and mindfulness can help manage the emotional distress.
- Engage in Health-Promoting Behaviors: Regular physical activity, a balanced diet, and adequate sleep can improve mood and resilience, making it easier to connect with others and buffer the physiological effects of stress.
Conclusion: Prioritizing Connection for a Healthier Life
The evidence is clear: the impact of loneliness on physical health markers is significant and far-reaching, from cardiovascular strain and chronic inflammation to impaired immunity and cognitive decline. Loneliness is not merely an emotional discomfort; it is a serious threat to our physical well-being, demanding attention from individuals, communities, and public health initiatives.
Prioritizing genuine social connection and actively addressing feelings of loneliness are not just about improving mental health; they are fundamental steps towards building a healthier, more resilient life, both individually and collectively. Embracing connection is an investment in our long-term physical health.



