Why Winter Worsens Psoriasis: The Science Behind the Flare-Ups
Understanding why winter exacerbates psoriasis is the first step toward effective prevention. Several environmental and physiological factors converge during the colder months, creating a perfect storm for skin irritation and inflammation.
Dry Air and Low Humidity
One of the primary culprits is the lack of humidity. Cold air naturally holds less moisture, and indoor heating systems further strip the air of hydration. This leads to dry skin, which can become itchy, cracked, and more prone to psoriatic lesions. The compromised skin barrier is less effective at protecting against irritants and infections.

Reduced Sun Exposure
Sunlight, specifically UVB rays, is a natural immunosuppressant and often helps improve psoriasis symptoms. During winter, shorter days and less time spent outdoors mean significantly reduced exposure to therapeutic UV light. This lack of natural phototherapy can trigger or worsen existing plaques.
Increased Stress and Illnesses
The holiday season, financial pressures, and general winter blues can elevate stress levels, a known trigger for psoriasis flares. Furthermore, winter is prime time for colds, flu, and other infections. Illnesses, especially those caused by streptococcal bacteria (like strep throat), are common triggers for guttate psoriasis and can worsen other forms.
Essential Strategies for Psoriasis Flare-Up Prevention in Winter
To successfully prevent psoriasis flare-ups in winter, a multi-faceted approach focusing on hydration, protection, and overall well-being is crucial. These strategies aim to counteract the harsh winter conditions and support your skin’s health.
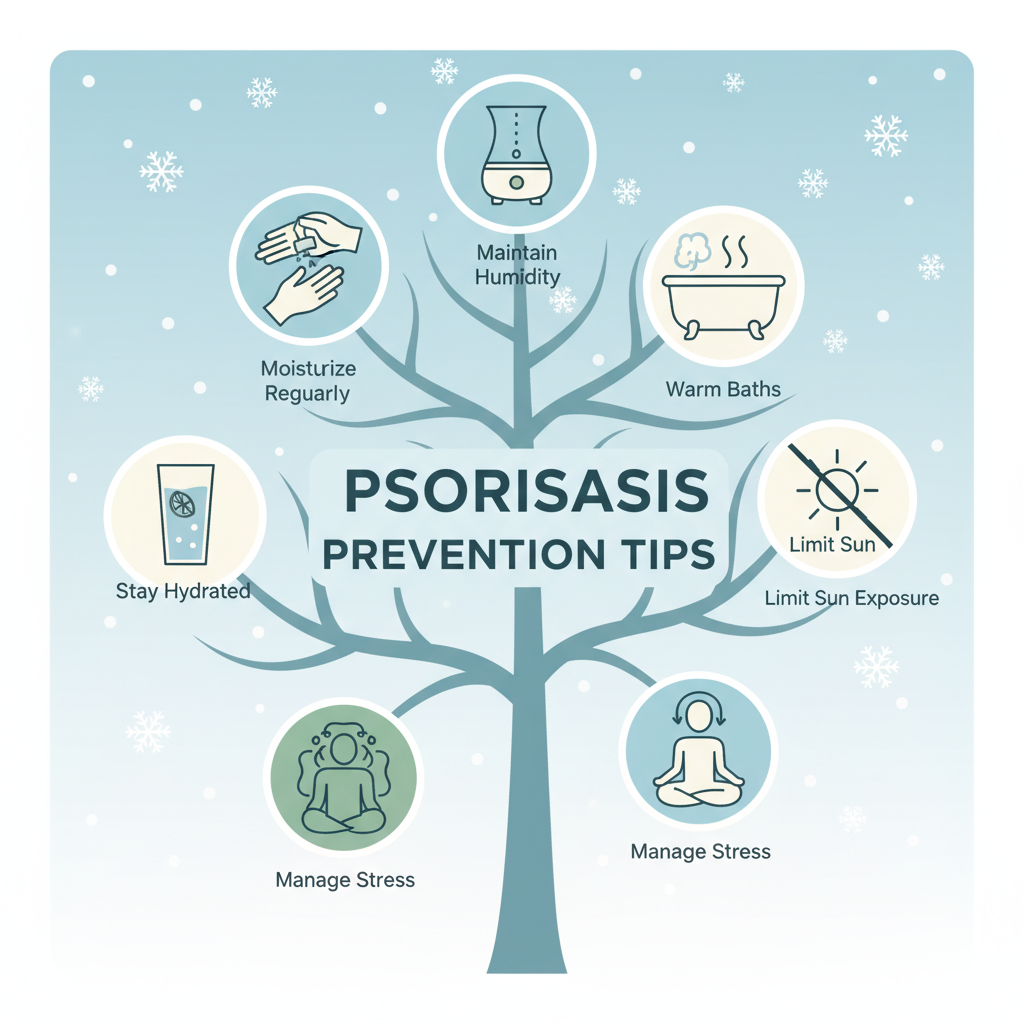
Master Your Moisturizing Routine
Moisturizing is arguably the most critical step in winter psoriasis management. Opt for thick, emollient-rich moisturizers, such as ointments or creams, rather than lotions, as they provide a more robust barrier. Apply moisturizer generously multiple times a day, especially immediately after bathing when skin is still damp, to lock in moisture effectively.
- **Choose the Right Product:** Look for fragrance-free, dye-free products formulated for sensitive skin. Ingredients like ceramides, hyaluronic acid, petrolatum, and mineral oil are excellent for hydration.
- **Frequent Application:** Apply moisturizer at least twice daily, and more often on affected areas or after washing your hands.
Embrace Humidifiers
Combat the dry indoor air by using a humidifier in your home, particularly in your bedroom while you sleep. A humidity level between 40-60% can significantly improve skin hydration and reduce dryness and itching. Remember to clean your humidifier regularly to prevent mold and bacteria growth.
Smart Bathing Habits
While a hot bath might feel comforting in winter, excessively hot water can strip your skin of its natural oils, leading to further dryness. Opt for lukewarm showers or baths lasting no more than 5-10 minutes. Use a gentle, fragrance-free cleanser instead of harsh soaps. After bathing, gently pat your skin dry with a soft towel and immediately apply your chosen moisturizer.
- **Oatmeal Baths:** Colloidal oatmeal baths can be soothing for itchy, inflamed skin.
- **Bath Oils:** Add emollients or bath oils to your bathwater to enhance hydration.
Protect Your Skin from the Elements
When venturing outdoors, shield your skin from cold winds and low temperatures. Wear gloves, scarves, and hats to cover exposed areas. Layering clothing made from soft, breathable fabrics like cotton can also help prevent irritation while keeping you warm.
Reconsider UV Exposure (Phototherapy)
If natural sunlight isn’t available, discuss phototherapy with your dermatologist. Controlled exposure to medical UV light can be an effective treatment during winter months to mimic the beneficial effects of the sun. Home phototherapy units are also an option for some patients, always under medical supervision.
Nurture Your Body from Within: Diet and Supplements
A balanced diet rich in anti-inflammatory foods can support overall skin health. Focus on fruits, vegetables, lean proteins, and healthy fats. Some supplements may also be beneficial.
- **Vitamin D:** Winter can lead to vitamin D deficiency due to reduced sun exposure. Discuss with your doctor whether a vitamin D supplement is appropriate, as it plays a role in immune function and skin health.
- **Omega-3 Fatty Acids:** Found in fatty fish, flaxseeds, and walnuts, omega-3s have anti-inflammatory properties that may benefit psoriasis.
- **Hydration:** Drink plenty of water throughout the day to keep your body and skin hydrated from the inside out.
Stress Management: A Key to Control
Stress is a well-known trigger for psoriasis flares. During the often-stressful winter months, prioritize stress-reducing activities. Incorporate practices like meditation, yoga, deep breathing exercises, spending time in nature, or engaging in hobbies you enjoy. Adequate sleep is also vital for stress reduction and overall immune health.
Regular Check-ups and Treatment Adherence
Maintain regular appointments with your dermatologist to review your treatment plan. Winter might necessitate adjustments to your medications or the introduction of new therapies to manage increased flare activity. Diligently follow your prescribed treatment regimen, whether it involves topical creams, oral medications, or biologics, as consistency is key to long-term control.
Lifestyle Adjustments for Winter Wellness
Beyond specific skin care, certain lifestyle choices can make a significant difference in preventing winter psoriasis flares.
Clothing Choices Matter
Opt for loose-fitting clothing made from soft, natural fibers like cotton to minimize friction and irritation on your skin. Wool can be irritating for some individuals. Layering allows you to adjust to temperature changes, preventing overheating and sweating, which can also irritate psoriatic skin.
Stay Hydrated
The importance of internal hydration cannot be overstated. Water helps maintain skin elasticity and overall bodily functions. Carry a water bottle and sip throughout the day, even if you don’t feel thirsty, especially if you spend a lot of time indoors with heating on.
Avoid Known Triggers
Pay close attention to anything that consistently triggers your psoriasis, which might become more pronounced in winter. Common triggers include alcohol, smoking, certain foods, or even specific medications. Identifying and avoiding these can significantly reduce flare frequency.
When to Seek Professional Help
Despite your best efforts, winter flares can sometimes be unavoidable or severe. If your psoriasis is significantly worsening, not responding to your current treatments, or impacting your quality of life, it is crucial to consult your dermatologist. They can assess your condition, adjust your treatment plan, and explore advanced therapies to help you navigate the colder months more comfortably.
Successfully navigating winter with psoriasis involves vigilance, consistency, and a deep understanding of your personal triggers. By adopting these comprehensive strategies for psoriasis flare-up prevention in winter, you can significantly reduce the impact of the season on your skin, allowing you to enjoy the colder months with greater comfort and confidence.


